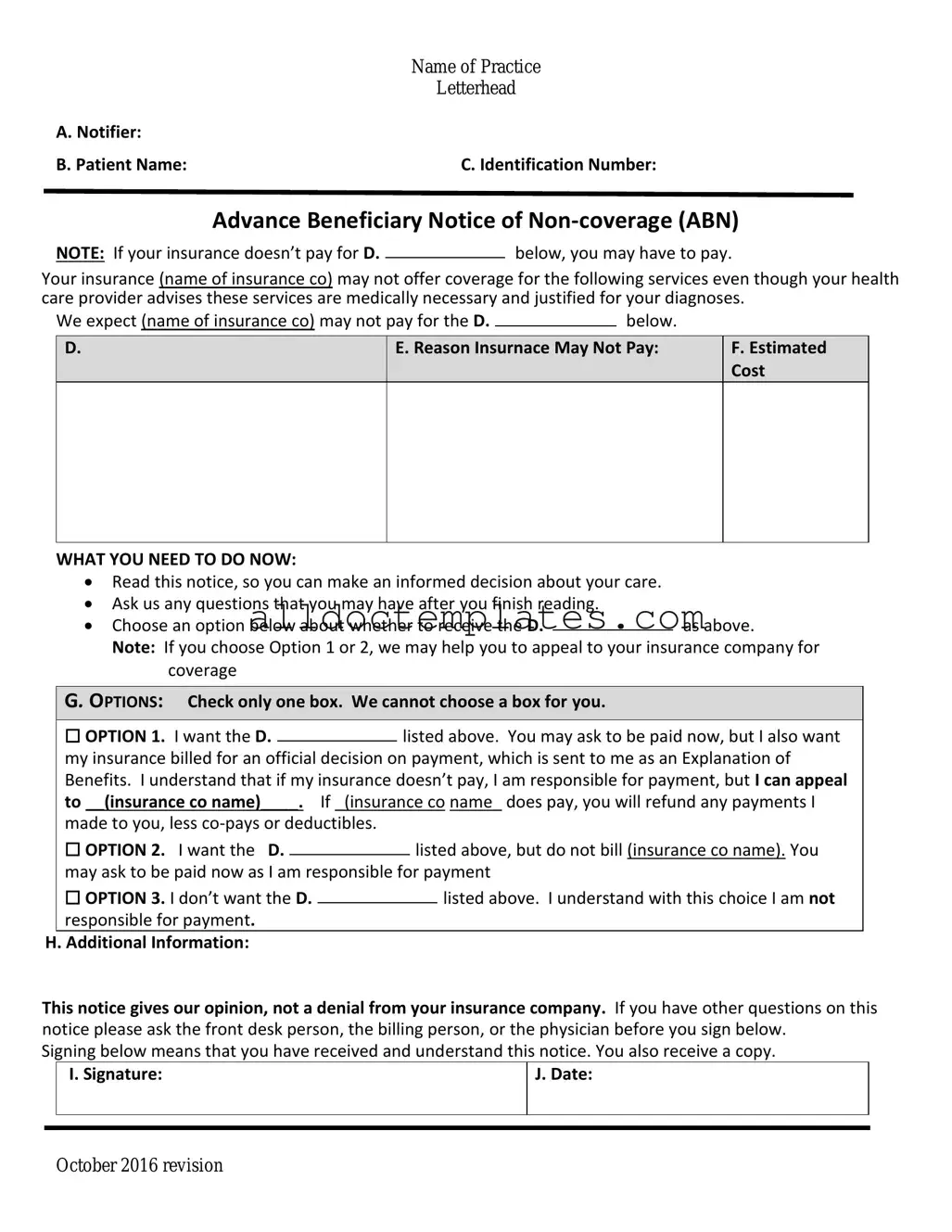
Fill in a Valid Advance Beneficiary Notice of Non-coverage Form
Document Sample
|
Name of Practice |
|
Letterhead |
A. Notifier: |
|
B. Patient Name: |
C. Identification Number: |
Advance Beneficiary Notice of
NOTE: If your insurance doesn’t pay for D.below, you may have to pay.
Your insurance (name of insurance co) may not offer coverage for the following services even though your health care provider advises these services are medically necessary and justified for your diagnoses.
We expect (name of insurance co) may not pay for the D. |
|
below. |
|
D.
E. Reason Insurnace May Not Pay:
F.Estimated Cost
WHAT YOU NEED TO DO NOW:
Read this notice, so you can make an informed decision about your care.
Ask us any questions that you may have after you finish reading.
Choose an option below about whether to receive the D.as above.
Note: If you choose Option 1 or 2, we may help you to appeal to your insurance company for coverage
G. OPTIONS: Check only one box. We cannot choose a box for you.
|
☐ OPTION 1. I want the D. |
|
listed above. You may ask to be paid now, but I also want |
||||
|
|
||||||
|
my insurance billed for an official decision on payment, which is sent to me as an Explanation of |
||||||
|
Benefits. I understand that if my insurance doesn’t pay, I am responsible for payment, but I can appeal |
||||||
|
to __(insurance co name)____. If _(insurance co name_ does pay, you will refund any payments I |
||||||
|
made to you, less |
|
|
|
|||
|
☐ OPTION 2. I want the D. |
|
|
listed above, but do not bill (insurance co name). You |
|||
|
|
|
|||||
|
may ask to be paid now as I am responsible for payment |
||||||
|
☐ OPTION 3. I don’t want the D. |
|
|
|
listed above. I understand with this choice I am not |
||
|
|
|
|
||||
|
responsible for payment. |
|
|
|
|||
H. Additional Information: |
|
|
|
||||
This notice gives our opinion, not a denial from your insurance company. If you have other questions on this notice please ask the front desk person, the billing person, or the physician before you sign below.
Signing below means that you have received and understand this notice. You also receive a copy.
|
I. Signature: |
J. Date: |
|
|
|
|
|
|
October 2016 revision
Document Information
| Fact Name | Description |
|---|---|
| Purpose | The Advance Beneficiary Notice of Non-coverage (ABN) informs Medicare beneficiaries that a service or item may not be covered by Medicare. |
| Requirement | Providers must issue an ABN when they believe Medicare will deny payment for a service, allowing patients to make informed decisions about their care. |
| Patient Rights | Beneficiaries have the right to refuse services after receiving the ABN, understanding that they may be responsible for the costs if Medicare does not cover the service. |
| State-Specific Laws | In some states, additional regulations may apply regarding the use of the ABN. For instance, California has specific guidelines under the California Code of Regulations. |
Advance Beneficiary Notice of Non-coverage - Usage Guidelines
After receiving the Advance Beneficiary Notice of Non-coverage (ABN), it is important to complete the form accurately. This will help ensure that you understand your financial responsibilities regarding the services you are about to receive.
- Begin by entering the date at the top of the form.
- Fill in your name and contact information in the designated fields.
- Provide the name of the healthcare provider or facility that issued the ABN.
- Clearly describe the services or items that you are being notified about.
- Indicate the reason the provider believes Medicare may not cover the services.
- Sign and date the form to confirm your understanding and acknowledgment.
- Keep a copy of the completed form for your records.
Common PDF Forms
Dh 680 Form Pdf - The Department of Health oversees the issuance and management of this certification.
The Colorado Mobile Home Bill of Sale is a legal document that facilitates the transfer of ownership of a mobile home from one party to another. This form outlines essential details such as the buyer and seller's information, the mobile home's description, and the sale price. For those seeking a reliable template, you can find a helpful resource at Colorado PDF Templates. Understanding this document is crucial for ensuring a smooth transaction and protecting the rights of both parties involved.
Letter of Intent to Purchase Land Pdf - It includes the potential for additional provisions related to legal aspects of the transaction.
Annual Physical Examination Form Pdf - Indicate if you take medications independently for safety tracking.
Dos and Don'ts
When filling out the Advance Beneficiary Notice of Non-coverage form, it’s important to be careful and thorough. Here are some key dos and don’ts to keep in mind:
- Do read the instructions carefully before starting.
- Do provide accurate information about the services received.
- Don't leave any required fields blank.
- Don't rush through the form; take your time to ensure everything is correct.
Common mistakes
-
Not reading the instructions carefully: Many individuals overlook the importance of understanding the guidelines provided with the form. This can lead to incomplete or incorrect information being submitted.
-
Failing to provide accurate patient information: It's crucial to ensure that the patient's name, Medicare number, and other identifying details are correct. Errors here can cause significant delays in processing.
-
Ignoring the service details: Some people forget to specify the services or items for which they are receiving the notice. This omission can create confusion and complicate the review process.
-
Not signing the form: A signature is often required to validate the notice. Without it, the form may be considered incomplete, resulting in unnecessary complications.
-
Neglecting to date the form: Failing to include the date can lead to questions about when the notice was issued. This detail is essential for establishing timelines.
-
Misunderstanding the implications: Some individuals do not fully grasp what the notice means for their coverage. This misunderstanding can lead to confusion about potential costs and responsibilities.
-
Not keeping a copy: After submitting the form, individuals often forget to keep a copy for their records. This can be problematic if questions arise later regarding the notice.
-
Overlooking the appeal process: Many fail to note the instructions for appealing a decision related to the notice. Understanding this process is vital for those who wish to contest a non-coverage determination.
-
Relying solely on verbal communication: Some individuals assume that discussing the notice with a provider is sufficient. However, written documentation is necessary to ensure clarity and accountability.